INFLAMMATION
RESOLUTION
A NEW THERAPEUTIC TARGET
Latest research including single-molecule transcriptome sequencing demonstrates how a multicomponent, multitarget treatment can potentially promote inflammation resolution and tissue healing. Read below to find out why this is clinically important and how to attend one of our forthcoming events.
Inflammation resolution is a critical process
Inflammation resolution is not merely a passive cessation of proinflammatory mechanisms. It is a complex, tightly regulated system of processes that is critical for tissue healing and restoration of function. Important elements include1–5:
- Neutrophil influx: swarming of neutrophils from the blood stream into the injury site
- Lipid mediator class switch: release of proresolving mediators, such as lipoxins, resolvins, protectins and maresins
- Efferocytosis: removal of exhausted, mainly apoptotic neutrophils to prevent tissue damage; many are removed by macrophages
- Macrophage phenotype switch: “reprogramming” triggered by efferocytosis, from a proinflammatory to a proresolution phenotype, contributing towards postresolution immune tolerance and prevention of autoimmunity
- Neutrophil phenotype switch: “reprogramming” to an anti-inflammatory type, promoting neutrophil reverse migration
- Neutrophil influx: swarming of neutrophils from the blood stream into the injury site
- Lipid mediator class switch: release of proresolving mediators, such as lipoxins, resolvins, protectins and maresins
- Efferocytosis: removal of exhausted, mainly apoptotic neutrophils to prevent tissue damage; many are removed by macrophages
- Macrophage phenotype switch: “reprogramming” triggered by efferocytosis, from a proinflammatory to a proresolution phenotype, contributing towards postresolution immune tolerance and prevention of autoimmunity
- Neutrophil phenotype switch: “reprogramming” to an anti-inflammatory type, promoting neutrophil reverse migration

Recently, an Atlas of Inflammation Resolution was created, providing the most detailed understanding of acute inflammation and inflammation resolution to date.
https://www.sbi.uni-rostock.de/research/projects/detail/62
Treatments that suppress inflammation may also suppress its resolution
In severe conditions, an anti-inflammatory strategy is mandatory to prevent tissue destruction or an overwhelming inflammatory process. Alternatively, a proresolution strategy could be considered the treatment of choice.6
Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibiting the cyclooxygenase-2 (COX-2) pathway are a mainstay of inflammation treatment. COX-2 promotes biosynthesis of many proinflammatory mediators, but some are equally important for initiation of inflammation resolution.2
- A lipid mediator class switch2
- A macrophage phenotype switch2
- A neutrophil phenotype switch7
Abbreviations: COX, cyclooxygenase; LOX, lipoxygenase; LTs, leukotrienes; PGs, prostaglandins; PGE2, prostaglandin E2; SPMs, specialized proresolving mediators.
NSAID treatment may have beneficial effects in the early phase of inflammation by preventing prostanoid production, but may also be “resolution-toxic,” by disrupting the production of anti-inflammatory prostaglandins and lipoxins.2
Multitarget drugs provide a better solution for complex processes like inflammation resolution
Abbreviations: COX-2, cyclooxygenase 2; PGE2, prostaglandin E2.
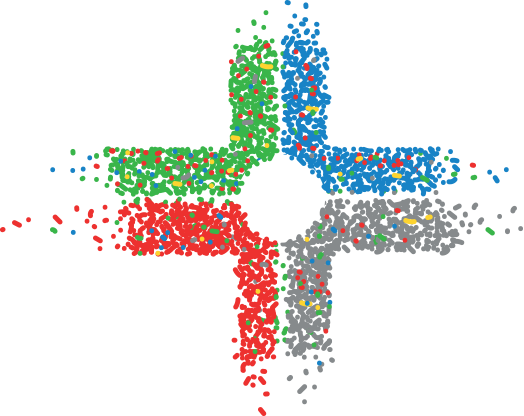
- Single-target drugs are designed to target a single biological entity (usually a protein) with high selectivity, not taking interactions with other targets into consideration
- Due to network complexity of disease biology, single-target drugs may have unwanted “ripple” effects on other “off-target” entities
- These “ripple” effects can potentially cause side effects, limiting the effective dose and effectiveness of the single-target drug
Abbreviations: COX-2, cyclooxygenase 2; FPR2, formyl peptide receptor 2; LTB4, leukotriene B4; LTAH, leukotriene A4 hydrolase; LXA4, lipoxin A4; PGE2, prostaglandin E2.
- Multitarget drugs can target a larger part of the signaling network
- They can balance signaling inhibition with promotion by targeting selected synergistic pathways
- The synergistic effect of multiple targets across the signaling network allows to reduce pharmacological doses and possible side effects
Abbreviations: COX-2, cyclooxygenase 2; FPR2, formyl peptide receptor 2; LTB4, leukotriene B4; LTAH, leukotriene A4 hydrolase; LXA4, lipoxin A4; PGE2, prostaglandin E2.
- Single-target drugs are designed to target a single biological entity (usually a protein) with high selectivity, not taking interactions with other targets into consideration
- Due to network complexity of disease biology, single-target drugs may have unwanted “ripple” effects on other “off-target” entities
- These “ripple” effects can potentially cause side effects, limiting the effective dose and effectiveness of the single-target drug
- Multitarget drugs can target a larger part of the signaling network
- They can balance signaling inhibition with promotion by targeting selected synergistic pathways
- The synergistic effect of multiple targets across the signaling network allows to reduce pharmacological doses and possible side effects
Traumeel has a well-established
efficacy and safety profile
In vitro
- Complex regulation of the inflammation process (granulocytes, lymphocytes, platelets and endothelial cells)8
In vivo
- Acute and chronic inflammation, edema (swelling and local inflammation)9,10
- Gene expression changes in inflammation (wound-healing model)11
Clinical vs placebo
- Acute sprains of the ankle12
- Acute musculoskeletal injuries13
- Knee osteoarthritis (+ Zeel T)14
Clinical vs NSAIDs
- Vs diclofenac gel15, 16 and injectable NSAIDs17
- Tendinopathy,16 epicondylitis17 and injuries of various origins15
- Complex regulation of the inflammation process (granulocytes, lymphocytes, platelets and endothelial cells)8
- Acute and chronic inflammation, edema (swelling and local inflammation)9, 10
- Gene expression changes in inflammation (wound-healing model)11

- Acute sprains of the ankle12
- Acute musculoskeletal injuries13
- Knee osteoarthritis
(+ Zeel T)14
- Vs diclofenac gel15,16 and injectable NSAIDs17
- Tendinopathy,16 epicondylitis17 and injuries of various origins15
Traumeel has demonstrated effects on the mediators and cells involved in inflammation resolution
Abbreviations: COX-2, cyclooxygenase 2; IL-1β, interleukin 1β; IL-10, interleukin 10; LTB4, leukotriene B4; MMP13, matrix metalloproteinase 13; NF-κΒ, nuclear factor κΒ; PGD2, prostaglandin D2; TNF-α, tumor necrosis factor α; TGF-β, transforming growth factor β.
Forthcoming events
REFERENCES
- Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014;510(7503):92-101. doi:10.1038/nature13479.
- Sugimoto MA, Sousa LP, Pinho V, Perretti M, Teixeira MM. Resolution of inflammation: what controls its onset? Front Immunol. 2016;7:160. doi:10.3389/fimmu.2016.00160.
- Feehan KT, Gilroy DW. Is resolution the end of inflammation? Trends Mol Med. 2019;25(3):198-214. doi:10.1016/j.molmed.2019.01.006.
- Jones HR, Robb CT, Perretti M, Rossi AG. The role of neutrophils in inflammation resolution. Semin Immunol. 2016;28(2):137-145. doi:10.1016/j.smim.2016.03.007.
- De Oliveira S, Rosowski EE, Huttenlocher A. Neutrophil migration in infection and wound repair: going forward in reverse. Nat Rev Immunol. 2016;16(6):378-391. doi:10.1038/nri.2016.49.
- Fullerton JN, Gilroy DW. Resolution of inflammation: a new therapeutic frontier. Nat Rev Drug Discov. 2016;15(8):551-567. doi:10.1038/nrd.2016.39.
- Loynes CA, Lee JA, Robertson AL, et al. PGE2 production at sites of tissue injury promotes an anti-inflammatory neutrophil phenotype and determines the outcome of inflammation resolution in vivo. Sci Adv. 2018;4(9):eaar8320. doi:10.1126/sciadv.aar8320.
- Cesnulevicius K. The bioregulatory approach to work-related musculoskeletal disorders: using the multicomponent ultra low-dose medication Traumeel to target the multiple pathophysiological processes of the disease. Altern Ther Health Med. 2011;17(suppl 2):S8-S17.
- Lussignoli S, Bertani S, Metelmann H, Bellavite P, Conforti A. Effect of Traumeel S, a homeopathic formulation, on blood-induced inflammation in rats. Complement Ther Med. 1999;7(4):225-230. doi: 10.1016/S0965-2299(99)80006-5.
- Conforti A, Bertani S, Metelmann H, Chirumbolo S, Lussignoli S, Bellavite P. Experimental studies on the anti-inflammatory activity of a homeopathic preparation. Biomed Ther. 1997;15(1):28-31.
- St. Laurent G III, Seilheimer B, Tackett M, et al. Deep sequencing transcriptome analysis of murine wound healing: effects of a multicomponent, multitarget natural product therapy-Tr14. Front Mol Biosci. 2017;4:57. doi:10.3389/fmolb.2017.00057.
- Zell J, Connert WD, Mau J, Feuerstake G. Treatment of acute sprains of the ankle: a controlled double-blind trial to test the effectiveness of a homeopathic ointment. Biol Ther. 1989;7(1):1-6.
- Böhmer D, Ambrus P. Treatment of sports injuries with Traumeel ointment: a controlled double-blind study. Biol Ther. 1992;10(4):290-300.
- Lozada CJ, del Rio E, Reitberg DP, Smith RA, Kahn CB, Moskowitz RW. A double-blind, randomized, saline-controlled study of the efficacy and safety of co-administered intra-articular injections of Tr14 and Ze14 for treatment of painful osteoarthritis of the knee: the MOZArT trial. Eur J Integr Med. 2017;13:54-63. doi:10.1016/j.eujim.2017.07.005.
- González de Vega C, Speed C, Wolfarth B, González J. Traumeel vs. diclofenac for reducing pain and improving ankle mobility after acute ankle sprain: a multicentre, randomised, blinded, controlled and non-inferiority trial. Int J Clin Pract. 2013;67(10):979-989. doi:10.1111/ijcp.12219.
- Schneider C, Klein P, Stolt P, Oberbaum M. A homeopathic ointment preparation compared with 1% diclofenac gel for acute symptomatic treatment of tendinopathy. Explor J Sci Heal. 2005;1(6):446-452. doi:10.1016/j.explore.2005.08.010.
- Birnesser H, Oberbaum M, Klein P, Weiser M. The homeopathic preparation Traumeel S compared with NSAIDs for symptomatic treatment of epicondylitis. J Musculoskelet Res. 2004;8(2 & 3):119-128. doi:10.1142/S0218957704001284.
© 2020 Biologische Heilmittel Heel GmbH – All rights reserved | Legal Notice | Privacy Policy
